Involuntary movements with fever
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan. is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
Navyatha 110 ,( the patient's collateral relatives provided the history as the patient couldn't talk)
4th December: reduced altered sensorium
70 year old female,resident of miryalaguda came with
Chief complaints:
History of fever since 4 days
Involuntary movements on since 2day
Confusion,agitation since 1day
History of presenting illness:
Patient was asymptomatic 4 days back, and developed high grade fever which was gradual in onset and was intermittent type and this was associated with chills and rigors
This was associated with vomiting which was non projectile,non blood stained, contents with undigested food with mild abdominal pain,and there wasrelief after emesies
She was then taken to a local RMP was given I.v fluids and was diagnosed with dengue and was treating the hospital for the same
Then patient developed Involuntary movements of upper and lower limbs which was abrupt in onset and was associated with altered mental status
There was no association of intoxication, environmental exposure to toxins,headache, no recent change in medication
Patient's daily routine:
Patient would wake up everyday at 7:00 in the morning, and do her everyday rituals ,then she would have her breakfast which is mostly dal and rice .
Patient used to work in the farm fields 10 years back and stopped now because of her age
She now passes her time watching television and then has her lunch at 2pm followed by a short nap in the afternoon
She has her dinner at 8pm and goes to sleep by 9pm
The following are her the past reports:
Past history:
No similar complaints in the past
No history of hypertension, diabetes, Tuberculosis, seizures
Marital history:
Married at age 20 ,had her first child at25 2nd and 3rd at 28 and 30 age respectively.
Delivery by normal delivery
Surgical history:
Underwent tubectomy at age 34
Cataract surgery 1year back
Family history:
No significant family history
Personal history:
Diet:
mixedDiet, consumes rice on daily basis ,chicken and other non vegetarian foods occasionally
Appetite: normal
Sleep: adequate
Bowel and bladder habits :normal
Addictions:smoker(chutta) since 30 years stopped 1 year ago,toddy Consumption stopped 20 years
General examination:
Patient is conscious,coherent and Cooperative well oriented with time palce and person
No signs of pallor, Icterus cyanosis,Clubbing,Lymphadenopathy
Vitals:
Temperature: 37 .7
Bp:110/80mmhg
Pulse rate 70bpm
Respiratory Rate :18 cpm
Saturation:96
GCSscoring:
E3: eye opening to sound
V4 confused
M5 localized pain
Total:12
Head to toe examination:
Hair :normal
eyes :normal
ears :normal
no deviation of the mouth
Nails:no discoloration
Skin: pigmentation at certain areas
chest: normal , no scars
Abdomen:normal
spine: no deformity
Systemic examination:
CNS EXAMINATION
Higher mental functions:
Speech slurred
Consciousness:lethargy
Behavior:irritable
Spine:no deformity
Cranial nerve examination
1st nerve: olfactory normal
2nd optic nerve
Visual acuity: counting fingers
3rd 4th 6th nerve: oculomotor ,trochlear,abducens
Primary gaze present
EOM RT LT
SR n normal
IR normal
SO normal
IO normal
Ptosis absent
Pupils reactive to light
5th nerve RT LT
Corneal reflex + +
Jaw jerk + +
Sensation over the face-present
7thh nerve;
Frowning absent
Orbicularis oculi
Nasolabial fold present
8th nerve
Vestibular cochlear
Rt left
Rinnies + +
Webbers + +
9th nerve
Uvula central
10th nerve
Gag reflex present
Hypoglossal nerve
Symmetrical
Motor system
Muscle bulk
Muscle tone inspection
Palpation
Resistance seen on right upper limb
Power:
Grade 3 against gravity
Coordination movements normal
Finger nose test
Finger finger nose test
Involuntary movements present
Reflexes: Rt left
Corneal + +
Conjuctival
Palatial + +
Abdominal + +
Plantar + +
Deep Reflexes
Jaw jerk + +
Biceps jerk + ++
Supinator jerk ++
Triceps jerk + +
Knee jerk + +
Ankle jerk+ +
Sensory examination:
Fine touch present
Pain responding
Temperature felt
Vibration felt
Meaningealsigns:
Kerning sign positive
Brudzinikies sign
Neck stiffness
Investigation
Anti hcv
Altered sensorium secondary to hyponatremia?, viral dengue?( ns1+) meningo encephalitis?
Treatment:
O2 supplementation
Ryeles feeding
Inj dexa 8mg iv TID
NS 50ML/hr iv continuous infusion
Inj monocet 2g/iv BD
Discussion:
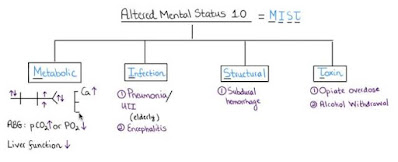
- Altered mental status may be classified according to its origin into 4 major groups: dementia, delirium, psychosis, and neurologic causes.
- Diagnostic criteria:
- By eliciting Reflexes
- Gcs
- Confusion Assessment Method for the ICU (CAM-ICU)
Reference: http://books.google.com/?id=c3I-(PFkMN2YC&pg=PA863&dq=%22level+of+consciousness%22)
adequate intravenous access, providing oxygen, and obtaining important vitals (e.g., temperature, respiratory rate, heart rate, BP, oxygen saturation, and blood sugar).
The following conditions must be identified and corrected promptly,
- HypotensionHypoglycemiaHypoxiaHypercapnia, andHyperthermia






































Comments
Post a Comment